Additional Credit
Among the important extras we offer as part of the Additional Credit are the following:
-
Site Tourism For The Patient & Attendant
-
Airport Pick & Drop Service
-
Ambulance service at airport
-
Priority appointments with The Doctor
-
Cancel Easily Anytime with Full Refund
-
Room Upgradation
-
Free Online Doctor Consultation Valued at USD 20
-
Free hotel Stay for 5 to 7 days Accordingly
-
Welcome Kit at Arrival
-
Interpreter
-
Medical Visa Assistance
What is Included?
- Doctor consultation charges
- Lab tests and diagnostic charges
- Room charges inside hospital during the procedure
- Surgeon Fee
- Cost of implant
- Nursing charges
- Hospital surgery suite charges
- Anesthesia charges
- Routine medicines and routine consumables (bandages, dressings etc.)
- Food and Beverages inside hospital stay for patient and one attendant.
What is not Included?
- Extra Radiology Investigations
- Healthcare Professionals Charges of other consultations.
- Other Requested Services such as Laundry etc.
- Additional Pharmaceutical Products and Medicines After Discharge from Hospital.
- Management of Conditions Unrelated to Procedures or Pre-Existing.
- The cost of any additional implants will be in addition to the package cost.
Package Description
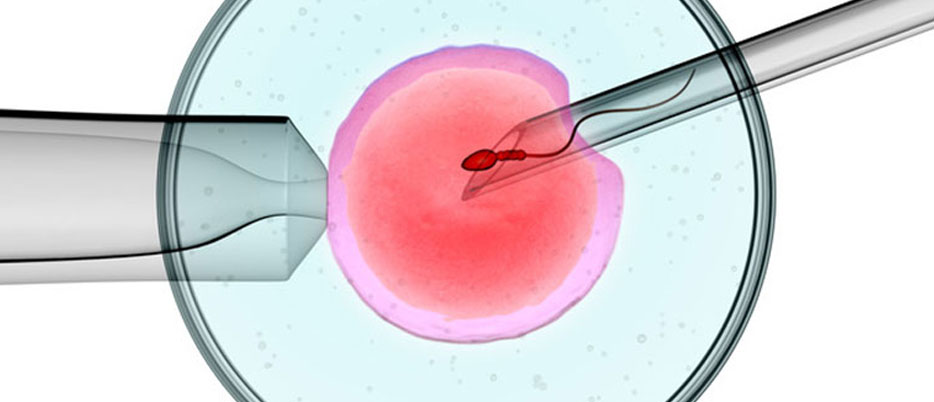
IMSI:
IMSI is a kind of ICSI in which sperm samples are analysed under a nearly 6000 times more powerful microscope to better determine their "morphology." The embryologist can see small flaws in the sperm head that would not be seen with regular ICSI at a greater magnification.
Before microinjecting, an IMSI test is used to distinguish between normal and abnormal sperm. It's done with a high-powered microscope and 600-fold digital imaging. During this process, the ultrastructure of the sperm is examined. The nucleus distortion is examined by the dermatologist.
IMSI (intracytoplasmic morphologically selected sperm injection) is a laboratory procedure for IVF treatments. It is an improved variant of ICSI in which high-quality sperm are inserted into the egg for fertilisation.
Disease Overview:
low sperm count
Low sperm count refers to the amount of sperm in the fluid (semen) you ejaculate after an orgasm.
Oligospermia is a term for a low sperm count. A total lack of sperm is referred to as azoospermia. If you have fewer than 15 million sperm per millilitre of sperm, your sperm count is considered poor.
Low sperm counts reduce the chances of one of your sperm fertilising your partner's egg and resulting in pregnancy. Despite this, many men with low sperm counts can nonetheless father a kid.
Disease Signs and Symptoms
The inability to conceive a child is the most common symptom of low sperm count. There may be no other visible symptoms or indicators. In some men, signs and symptoms may be caused by an underlying issue such as an inherited chromosomal defect, a hormonal imbalance, dilated testicular veins, or a disease that prevents sperm from passing through.
Symptoms of a low sperm count include:
- Low sex desire or difficulties sustaining an erection are examples of sexual function issues (erectile dysfunction)
- In the testicular region, there may be pain, swelling, or a lump.
- Reduced face or body hair, as well as other chromosomal or hormone abnormalities
Disease Causes:
The testicles (testes) as well as the hypothalamus and pituitary glands — structures in your brain that create hormones that activate sperm production — must all operate normally for sperm to be produced. When sperm are created in the testicles, they are transported through delicate tubes until they mingle with semen and are ejected from the penis. Any of these systems can have an impact on sperm production.
Anomalies in sperm form (morphology), movement (motility), or function can also occur.
However, the cause of low sperm count is frequently unknown.
Medical reasons
A low sperm count can be caused by a variety of medical conditions and therapies. Here are a few examples:
Varicocele. A varicocele is an enlargement of the veins draining the testis. It's the most prevalent cause of male infertility that can be reversed. Although the actual aetiology of infertility caused by varicoceles is uncertain, it may be linked to poor testicular temperature regulation. Varicoceles cause sperm to be of lower quality.
Infection. Some illnesses can affect sperm production or health, or induce scarring that prevents sperm from passing through. Some sexually transmitted illnesses, such as gonorrhoea or HIV, cause inflammation of the epididymis (epididymitis) or testicles (orchitis). Despite the fact that certain infections might result in irreversible testicular damage, sperm can usually be recovered.
Problems with ejaculation. Retrograde ejaculation happens when sperm enters the bladder instead of exiting from the tip of the urethra during orgasm.
Diabetes, spinal injuries, and bladder, prostate, or urethra surgery are all examples of health issues that can produce retrograde ejaculation or absence of ejaculation.
Certain drugs, such as blood pressure medications known as alpha blockers, might cause ejaculatory issues. Some ejaculatory issues can be corrected, while others are irreversible. Sperm may still be extracted directly from the testicles in most situations with persistent ejaculation issues.
Antibodies that target sperm are known as sperm antibodies. Anti-sperm antibodies are immune system cells that mistake sperm for hazardous intruders and try to eliminate them.
Tumors. Male reproductive organs can be affected directly by cancers and nonmalignant tumours, or indirectly through glands that release hormones associated to reproduction, such as the pituitary gland. Tumors can be treated with surgery, radiation, or chemotherapy.
Testicles that haven't descended. One or both testicles may fail to descend from the abdomen into the sac that typically holds the testicles during foetal development (scrotum). Men with this illness are more likely to have lower fertility.
Hormone imbalances are a common problem. Hormones produced by the brain, pituitary, and testicles are required for sperm production. Changes in these hormones, as well as those from other organs including the thyroid and adrenal gland, can cause sperm production to be impaired.
Tubule defects that carry sperm. Sperm is carried in a variety of tubes. They can be obstructed for a variety of reasons, including surgical accidental harm, past infections, trauma, or improper growth, such as in cystic fibrosis or other genetic disorders.
The testicle, the tubes that drain the testicle, the epididymis, the vas deferens, the ejaculatory ducts, and the urethra can all become blocked.
Defects in the chromosomes. Guy reproductive organs develop abnormally in inherited illnesses such Klinefelter's syndrome, in which a male is born with two X chromosomes and one Y chromosome instead of one X and one Y. Cystic fibrosis, Kallmann's syndrome, and Kartagener's syndrome are some of the other genetic disorders linked to infertility.
Celiac disease is a kind of gluten intolerance. Celiac disease is a digestive ailment characterised by gluten intolerance that can lead to male infertility. Adopting a gluten-free diet may help with fertility.
Medications in particular. Testosterone replacement treatment, long-term anabolic steroid usage, cancer drugs (chemotherapy), some antifungal and antibiotic medications, certain ulcer medications, and other pharmaceuticals can reduce male fertility and impede sperm production.
Surgical procedures performed previously Vasectomy, inguinal hernia repairs, scrotal or testicular operations, prostate surgeries, and big abdominal surgeries for testicular and rectal tumours, among other procedures, may prohibit you from having sperm in your ejaculate. In most situations, surgery can be used to either remove sperm from the epididymis and testicles or to reverse the obstructions.
The effects of the environment
Overexposure to some environmental components can alter sperm production or function, including:
- Chemicals used in industry. Long-term exposure to benzenes, toluene, xylene, herbicides, pesticides, organic solvents, painting materials, and lead may be a factor in low blood lead levels.
- Exposure to heavy metal. Infertility can also be caused by exposure to lead or other heavy metals.
- X-rays or radiation. Radiation can cause sperm production to decrease. Sperm production might take many years to recover to normal. Sperm production can be permanently impaired by strong amounts of radiation.
- The testicles are overheated. Sperm production and function are harmed by high temperatures. Although research is sparse and inconsistent, regular use of saunas or hot tubs may reduce sperm count briefly.
- Sitting for lengthy amounts of time, wearing tight clothes, or working on a laptop computer for long lengths of time can all raise scrotal temperature and limit sperm production.
Causes include health, lifestyle, and other factors.
Drug usage is one of the other causes of low sperm count. Anabolic steroids, which are used to increase muscle strength and development, can shrink the testicles and reduce sperm production. Cocaine or marijuana use may also affect the quantity and quality of your sperm.
- Use of alcoholic beverages. Alcohol use lowers testosterone levels and reduces sperm production.
- Occupation. Certain jobs, such as welding and those that require extended sitting, such as truck driving, may increase the chance of infertility. However, the evidence for these connections is inconclusive.
- Tobacco consumption. Men who smoke may have lower sperm counts than men who do not smoke.
- Emotional tension. Severe or long-term emotional stress, such as anxiety over fertility, may interfere with hormone production.
- Depression. Depression can have a deleterious impact on sperm concentration.
- Weight. Obesity can affect male fertility in a variety of ways, including directly affecting sperm and generating hormone changes that lower male fertility.
- Problems with sperm testing: Testing a sperm sample that was collected too soon after your previous ejaculation, too soon after a sickness or stressful event, or didn't include all of the semen you ejaculated because some was spilled during collection might result in lower than normal sperm counts. As a result, most outcomes are based on many samples obtained over a period of time.
Risk Factors
Low sperm count and other disorders that might cause low sperm count are connected to a variety of risk factors. They are as follows:
- Tobacco smoking
- Using some illegal substances
- Being overweight is a problem.
- Being unhappy or worried to the point of exhaustion
- Having had or currently having certain infections
- Having to deal with toxins
- Testicles that have been overheated
- Having been through a testicular trauma
- Being born with a reproductive issue or having a blood family with a fertility disorder, such as your brother or parent
- Having specific medical issues, such as tumours or long-term diseases
- Having to go through cancer treatments such as radiation
- Using some prescription drugs
- Having had a vasectomy or other significant abdominal or pelvic surgery in the past
- Having a history of testicles that haven't descended
- consuming alcoholic beverages
Disease Diagnosis:
When you go to the doctor because you can't get your partner pregnant, he or she will try to figure out what's causing the problem. Even if your doctor feels your low sperm count is the issue, it's a good idea to get your spouse checked to rule out any other possible causes and see whether assisted reproductive treatments are needed.
Medical history and a general physical examination
Examining your genitals and asking questions about any genetic disorders, chronic health issues, illnesses, injuries, or operations that may impair your fertility are all part of this process. Your physician may also inquire about your sexual habits and growth.
Analyze the sperm
A semen analysis test is used to determine a low sperm count. Sperm count is usually assessed by looking at sperm under a microscope and counting how many sperm appear in squares on a grid pattern. A computer may be used to calculate sperm count in some instances.
Samples of sperm can be collected in a variety of methods. By masturbating and ejaculating into a designated container in the doctor's office, you may submit a sample. Some males prefer an alternate technique of sperm collecting due to religious or cultural beliefs. In such instances, semen can be collected during intercourse by using a specific condom.
In the testicles, new sperm are constantly created and mature in 42 to 76 days. As a result, a current semen study represents your three-month surroundings. Any beneficial adjustments you've made will take months to manifest.
Incomplete or incorrect sperm collection is one of the most prevalent reasons of low sperm count. Sperm numbers fluctuate a lot. Because of these considerations, most doctors will compare two or more semen samples over time to guarantee consistency.
To guarantee that a collection is accurate, your doctor will:
When you ejaculate, be sure that all of your semen makes it into the collecting cup or collection condom.
Have you gone two to seven days without ejaculating before obtaining a sample?
After the initial sample, take a second one at least two weeks later.
Have you avoided using lubricants since they might impair sperm motility?
The findings of the sperm analysis
Sperm densities in normal males varies from 15 million to more than 200 million per millilitre of sperm. If you have less than 15 million sperm per millilitre or less than 39 million sperm overall per ejaculate, you have a low sperm count.
With lower sperm counts, your chances of getting your spouse pregnant diminish. Some males have no sperm at all in their sperm. This is referred to as azoospermia.
The amount of sperm in your sperm is just one of several elements that go into conception. Some guys who have low sperm counts are able to have children. Similarly, some men with normal sperm counts are unable to become fathers. Other elements, such as good sperm mobility, are needed to establish a pregnancy even if you have enough sperm (motility).
Other examinations
Your doctor may offer more testing to determine the reason of your low sperm count and other probable causes of male infertility based on the first findings. These can include the following:
Ultrasound of the scrotum. The testicles and supporting structures are examined using high-frequency sound waves.
Hormone testing is a procedure that involves measuring hormone levels. A blood test to evaluate the level of hormones generated by the pituitary gland and testicles, which play a critical role in sexual development and sperm production, may be recommended by your doctor.
Urinalysis after ejaculation. Sperm in your pee indicates that your sperm are moving backwards into your bladder during ejaculation instead of out your penis (retrograde ejaculation).
Genetic testing are available. When sperm concentration is abnormally low, genetic factors may be at play. A blood test can detect tiny alterations in the Y chromosome, which might indicate a genetic problem. To identify numerous congenital or hereditary disorders, genetic testing may be conducted.
Biopsy of the testicles. A needle is used to remove samples from the testicle in this test. The findings of a testicular biopsy can be used to determine whether or not sperm production is normal. If that's the case, a blockage or another issue with sperm movement is most likely to blame. However, this test is only utilised in specific circumstances and is seldom used to determine the reason of infertility.
Anti-sperm antibody tests are a type of test that looks for antibodies against sperm. These tests, which look for immune cells (antibodies) that target sperm and impair their capacity to function, aren't widely utilised.
Biopsy of the testes Using a needle, samples are taken from the testicle. If sperm production is normal, the findings of the testicular biopsy can be used to determine this. If that's the case, a blockage or other sperm transport issue is most likely to blame. However, this test is seldom utilised to detect the reason of infertility and is only used in specific instances.
Antibody testing for sperm. These tests, which look for immune cells (antibodies) that target sperm and impair their capacity to function, are not widely utilised.
Disease treatment:
Low sperm count can be treated using a variety of methods, including:
Surgery. A varicocele, for example, can frequently be surgically rectified, as can a blocked vas deferens. Vasectomies that have already been performed can be reversed. When there are no sperm in the ejaculate, sperm retrieval procedures can frequently be used to get sperm straight from the testicles or epididymis.
Infection treatment. Antibiotics can treat a reproductive tract infection, but they don't always restore fertility.
Treatments for issues in sexual intercourse. In cases of erectile dysfunction or premature ejaculation, medication or counselling might assist increase fertility.
Treatments and drugs for hormones. In situations when infertility is caused by high or low levels of specific hormones, or difficulties with the way the body processes hormones, your doctor may suggest hormone replacement or drugs.
Aspects of assisted reproduction technology (ART). Depending on your personal condition and preferences, ART treatments may include collecting sperm by regular ejaculation, surgical extraction, or from donor persons. After that, the sperm are either injected into the female vaginal canal or utilised for IVF or intracytoplasmic sperm injection.
Information related to Treatment
Package Details
Days in Hospital
7 Days
Days in Hotel
*
30 Days
Room Type
Private

Treating Doctor
Dr. Ajantha Boopathi
IVF and Infertility Specialist- IVF Specialist, Male Infertility
Nova IVF Centre and Fertility Clinic, Anna Nagar, Chennai Chennai, India
15 Years of Experience

Treating Doctor
Dr. Surveen ghumman sindhu
IVF and reproductive medicine specialist- Infertility Specialist, IVF Specialist, Infertility Specialist, IVF Specialist, General Surgery, Hysterectomy (Abdominal/Vaginal), Fibroid Removal Surgery, Laparoscopic Abdominal Hysterectomy, Polycystic Ovarian Syndrome (PCOS) Treatment, General Surgery, Gynecology, Hysterectomy (Abdominal/Vaginal), General Surgery
Max Super Speciality Hospital New Delhi, India
32 Years of Experience

Treating Doctor
Dr. Richa Jagtap
IVF and Infertility Specialist- High risk pregnancy, Intra-Uterine Insemination (IUI), ICSI, ICSI, Colposcopy, ICSI, Female infertility, Infertility Treatment, In-vitro fertilization (IVF), Gynae endoscopy and Laparoscopic Myomectomy., Pre and Post Delivery Care, Colposcopy, Adiana System
ART Fertility Clinics, Mumbai Mumbai, India
27 Years of Experience

Treating Doctor
Dr. Anuradha kapur
Obstetrician and gynecologist- High risk pregnancy, IVF, IVF, Polycystic Ovarian Syndrome (PCOS) Treatment, IVF, Mild Endometriosis, Fibroid Removal, Painless Deliveries, Gynae endoscopy and Laparoscopic Myomectomy., High Blood Pressure and Diabetes in Pregnency, Intra Cystoplasmic sperm injection and IUI, High risk obstetrics, Reproductive endocrinology and Infertility
Max Super Speciality Hospital New Delhi, India
30 Years of Experience

Treating Doctor
Dr Neeta Gupta
IVF and reproductive medicine specialist- High risk pregnancy, Caesarean Section (C Section), Normal Vaginal Delivery (NVD), Maternal Care/ Checkup, Obstetrics / Antenatal Care, Caesarean Section (C Section), Laparoscopic Surgery (Obs & Gyn), Caesarean Section (C Section), Normal Vaginal Delivery (NVD), Obstetrics / Antenatal Care
Fortis Hospital Noida Noida, India
21 Years of Experience

Treating Doctor
Dr Kavita C Katoch
Obstetrician and gynecologist- Infertility Specialist, IVF Specialist, Infertility Specialist, IVF Specialist, Abortion and MTP, Endometriosis, High risk pregnancy, Caesarean Section (C Section), Intra-Uterine Insemination (IUI), ICSI, ICSI, Ovarian Cyst Removal, ICSI, Hysteroscopy, TESA, MESA, Polycystic Ovarian Syndrome (PCOS) Treatment, Endometriosis, Caesarean Section (C Section), Caesarean Section (C Section), Hysteroscopy, Endometriosis, Ovarian Cyst Removal, Heavy Periods, NPD, Percutaneous Epididymal Sperm Aspiration (PESA), Child Immunization, ERA, TESA, TESE, UTI Treatment
Fortis Flt. Lt. Rajan Dhall Hospital, Vasant Kunj, Delhi New Delhi, India
35 Years of Experience

Treating Doctor
Dr. Nandita Palshetkar
IVF and Infertility Specialist- Women's health, Hysterectomy (Abdominal/Vaginal), Delivery Procedure, Cesarean Section Procedure, Treatment Of Female Sexual Problems, Treatment Of Pregnancy Problems, Hysterectomy (Abdominal/Vaginal), Allopathy Treatment
Fortis Memorial Research Institute Gurgaon, India
36 Years of Experience

Treating Doctor
Dr. Hrishikesh D Pai
IVF and Infertility Specialist- Laparoscopic surgeon, Infertility Specialist, IVF Specialist, Infertility Specialist, IVF Specialist, Test Tube Baby, IUI Specialist, IUI Specialist, Blastocyst Culture and Transfer, ICSI, IVF with Donor Eggs, Laser Assisted Hatching (LAH), Surrogacy, Hysteroscopic Surgeon, ICSI, Test Tube Baby, ICSI, Surrogacy, Cryopreservation, Egg Freezing, Semen Freezing, Embryo Donation, Blastocyst Transfer, IMSI, TESA, Embryo Freezing (Slow Freezing & Vitrification), Microsurgical Epididymal Sperm Aspiration (MESA), TESA, TESE, Surrogacy
Fortis Memorial Research Institute Gurgaon, India
33 Years of Experience
Treating Doctor
Dr. Manish Banker
IVF and Infertility Specialist- Reproductive medicine, Reproductive endocrinology and Infertility
Nova IVF Centre and Fertility Clinic, Navrangpura, Ahmedabad Ahmedabad, India
28 Years of Experience

Treating Doctor
Dr. Shilpa Saple
IVF and Infertility Specialist- Intra-Uterine Insemination (IUI), Gynaecological Endoscopy, Blastocyst Culture and Transfer, ICSI, Surrogacy, ICSI, ICSI, Surrogacy, Embryo Donor Program, In-vitro fertilization (IVF), Gynaecological Endoscopy, Genetic counseling services, Surrogacy
ART Fertility Clinics, Mumbai Mumbai, India
22 Years of Experience