CORNEAL AND OCULAR SURFACE PROCEDURES-Scleral graft for scleral melting/perforation
India
-
Our Price USD 1684
-
Hospital Price USD 1773
-
You Save : USD 89
Booking Amount: USD 168. Pay Remaining 90% at the hospital.
Book NowAdditional Credit
Among the important extras we offer as part of the Additional Credit are the following:
-
Site Tourism For The Patient & Attendant
-
Airport Pick & Drop Service
-
Ambulance service at airport
-
Priority appointments with The Doctor
-
Cancel Easily Anytime with Full Refund
-
Room Upgradation
-
Free Online Doctor Consultation Valued at USD 20
-
Free hotel Stay for 5 to 7 days Accordingly
-
Welcome Kit at Arrival
-
Interpreter
-
Medical Visa Assistance
What is Included?
- Doctor consultation charges
- Lab tests and diagnostic charges
- Room charges inside hospital during the procedure
- Surgeon Fee
- Cost of implant
- Nursing charges
- Hospital surgery suite charges
- Anesthesia charges
- Routine medicines and routine consumables (bandages, dressings etc.)
- Food and Beverages inside hospital stay for patient and one attendant.
What is not Included?
- Extra Radiology Investigations
- Healthcare Professionals Charges of other consultations.
- Other Requested Services such as Laundry etc.
- Additional Pharmaceutical Products and Medicines After Discharge from Hospital.
- Management of Conditions Unrelated to Procedures or Pre-Existing.
- The cost of any additional implants will be in addition to the package cost.
Package Description
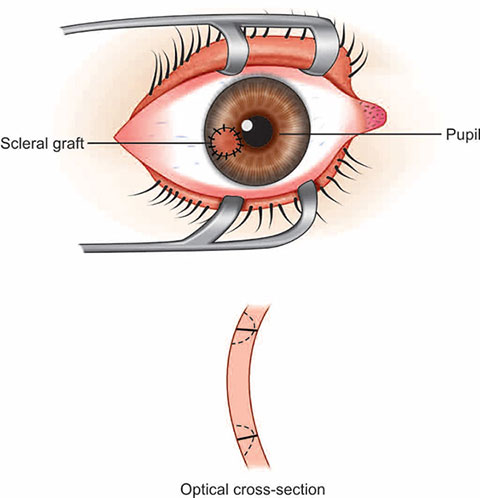
CORNEAL AND OCULAR SURFACE PROCEDURES-Scleral graft for scleral melting/perforation
Scleral grafting with an overlaying conjunctival or amniotic membrane graft is a straightforward and successful way to maintain globe structural and functional integrity. Because it is sturdy, flexible, easy to handle, and may be placed on host sclera, a scleral graft has been used to treat perforated corneal ulcers, scleral melting, or scleromalacia. A scleral graft can also be utilised to close an Ota nevus cosmetically.
Although scleral melt is a rare consequence of STAI, early detection and care of any predisposing factors, as well as surgical debridement, should be regarded as a key treatment option to save the eye.
Disease Overview:
Scleromalacia
The sclera develops yellow to grey spots that gradually produce a necrotic slough or sequestrum that finally separates from the underlying sclera, leaving naked choroid covered by a thin coating of fibrous tissue or conjunctiva.
Disease Signs and Symptoms:
- Astigmatism is a condition in which a person's (changes in the eye shape)
- Staphyloma is a kind of cancer (bulging at the weak point in the eyeball)
- Uveitis anterior (inflammation of the middle layer of the eye, called the uvea)
- Cataracts are a kind of cataract (clouding of the eye)
- Glaucoma is a disease that affects the eyes (increased inner eye pressure)
Disease Causes:
Other illnesses that can induce scleromalacia include systemic connective tissue diseases (most often rheumatoid arthritis) and inflammatory processes like vasculitis or infection; local damage to the sclera can also be a trigger.
Disease Diagnosis:
Scleromalacia perforans is diagnosed by an ophthalmologist using a slit lamp examination and a physical examination of the eye (a microscope that visualises the interior of the eye with a high-intensity light beam). The quantity and size of blood vessels in the back of the eye are usually reduced under the slit light, giving the tissues an almost porcelain-white look.
Disease Treatment:
Scleromalacia perforans is difficult to cure, especially because it is frequently discovered after the illness has progressed and irreversible eye damage has occurred. Nonetheless, several medicines may be able to reduce or stop the disease's course.
The following are some of the most regularly utilised treatments and procedures.
Nonsteroidal anti-inflammatory medicines (NSAIDs): Although scleromalacia perforans is not an inflammatory illness, many of its causes and effects are. NSAIDs such as Advil (ibuprofen), Ocufen (flurbiprofen), and Tivorbex (indomethacin) are among of the most regularly prescribed medications.
Immunomodulators: Because autoimmunity is a major cause of scleromalacia perforans, immunomodulators can be used to reduce the autoimmune response and limit disease development.
Cytoxan (cyclophosphamide), methotrexate, Imuran (azathioprine), and CellCept (mycophenolate mofetil) are among the options, as are biologics such Enbrel (etanercept), Remicade (infliximab), Rituxan (rituximab), and Kineret (kineret) (anakinra).
Topical agents include: Eye dryness, redness, and irritation are common symptoms of Scleromalacia perforans, and lubricating eye drops can help. Some doctors will administer sodium versenate eye drops to reduce shedding and prevent collagen degradation in the sclera (although the actual benefits of treatment remain unknown). Topical cyclosporin A is the same way.
Scleral graft surgery: In the rare case of worldwide perforation, surgery to repair the damaged region using scleral tissues from a transplant donor may be conducted.
Information related to Treatment
Package Details
Days in Hospital
1 Days
Days in Hotel
*
8 Days
Room Type
Private

Treating Doctor
Dr. Suraj Munjal
Ophthalmologist- Retina Surgeon, Cataract Surgeon, Lasik surgeon, Vitreo Retina Surgeon, Eyelid Surgery, Trabeculectomy, Vitreoretinal Surgery, Orbital & Oculoplastic surgery, Refractive surgery, Retina Examination, Glaucoma Evaluation / Treatment, Canaloplasty, Corneal Surgery, Eye Muscle Surgery, Orbital Surgery, Anterior Segment Surgery, Orbital Decompression Surgery for Thyroid Eye Disease, Orbital Trauma, Diabetic Retinopahy, YAG laser Posterior Capsulotomy, Anterior Retinal Cryotherapy, Retinal Surgery, Lens for Keratoconus
The Sight Avenue Eye Hospital Delhi, India
19 Years of Experience